Clostridiodes difficile (C. diff) is the leading cause of infectious diarrhea in healthcare settings, though clinical studies show that only 12-32% of hospitalized patients who develop diarrhea are due to C. diff, with less than 20% attributable to this bacterium. C. diff is present in feces and can spread to various surfaces, such as toilets, clothing, furniture, equipment, and hands. These bacteria can survive in the environment for long periods and be transmitted through contact with contaminated surfaces.
According to the National Institutes of Health, C. diff is naturally found in the digestive system of about one in 30 healthy adults. It can colonize the human gut harmlessly, as other “good” bacteria keep it in check. However, some antibiotics can disrupt this balance, eliminating the good bacteria and allowing C. diff to proliferate, leading to a C. diff infection (CDI). The bacteria cause nearly half a million CDI cases annually in the United States. Symptoms can range from mild, short-term diarrhea to severe cases causing dehydration and life-threatening damage to the colon.
In 2019, SSM Health St. Mary’s Hospital – Madison observed a sudden and significant increase in positive C. diff tests. To address this, the hospital initiated a study of its C. diff cases in collaboration with the Centers for Disease Control and Prevention and the American Hospital Association. Since watery diarrhea is a common symptom of C. diff, physicians often test for it in symptomatic patients. However, the test only confirms the presence of C. diff bacteria and not whether it is causing an active infection that requires antibiotic treatment. The hospital team suspected that many patients testing positive for C. diff were colonized rather than infected.
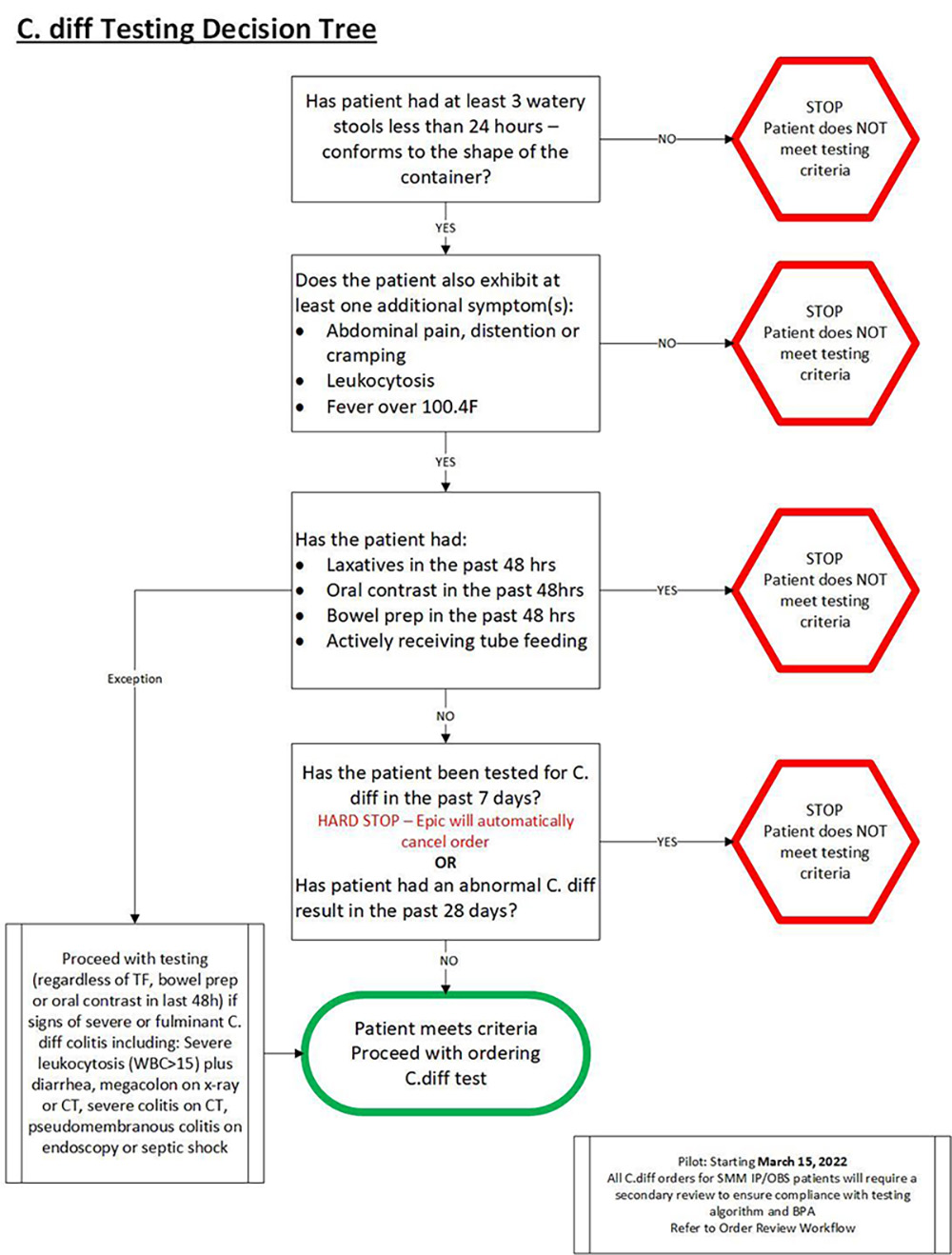
The hospital educated nurses and physicians on the full range of symptoms indicative of a C. diff infection, emphasizing that diarrhea alone is insufficient for diagnosis. Diarrhea can result from laxatives, antibiotics, oral contrast or bowel preparations, and tube feeding.They advised caregivers to look for additional symptoms such as abdominal pain, distention or cramping, fever over 100.4°F, nausea, anorexia, and leukocytosis before diagnosing CDI.
St. Mary’s Hospital also revised its best-practice C. diff algorithm to clarify the criteria for diagnosing CDI. In March 2022, they implemented a policy requiring automatic review by the hospital’s chief medical officer or regional hospitalist leader for all C. diff test orders. This review process involves assessing the patient's symptoms and consulting with the doctor before providing a second sign-off for testing.
This second sign-off procedure significantly reduced inappropriate testing and misdiagnosis of CDI. Treating colonized patients with antibiotics unnecessarily can increase the risk of true CDI infections, liver toxicity, and antimicrobial resistance. The success of this process has led to its adoption by six additional SSM Health hospitals in Wisconsin and throughout the organization’s four states.
Additionally, the St. Mary’s team enhanced infection prevention protocols, providing extensive education on hand hygiene, appropriate use of personal protective equipment, and cleaning hospital rooms and equipment with sporicidal agents like bleach to eliminate residual C. diff. Caregivers were instructed to notify unit managers immediately upon identifying patients with active CDI and to minimize transporting these patients within the hospital.
Through these comprehensive measures, St. Mary’s Hospital has effectively managed and reduced the incidence of C. diff infections, ensuring better patient outcomes and safety.