Implementation and Impact of Bedside Interdisciplinary Rounding
Background and Rationale: Interdisciplinary rounds are pivotal for comprehensive patient care, bringing together healthcare professionals to collaboratively determine the best treatment plans. At Western Wisconsin Health (WWH), the introduction of bedside interdisciplinary rounding became imperative post-COVID-19, aiming to mitigate communication challenges posed by pandemic protocols. By integrating bedside rounds, the focus was to foster communication, engagement, and shared decision-making between patients, caregivers, and the healthcare team.
Process and Implementation Timeline: The implementation process of bedside interdisciplinary rounding at WWH follows a structured approach ensuring comprehensive care planning, effective communication, and favorable patient health outcomes:
- Pre-Rounding Conference: The entire care team, including therapies, care management, respiratory therapists, dieticians, pharmacists, providers, and nurses, convene to discuss patient cases comprehensively, led by the assigned nurse.
- Bedside Rounds: The provider, primary nurse, and care coordinator or social worker then, visit the patient's bedside, facilitating direct communication and involving patients in their care.
- Identifying Barriers: The team addresses any identified barriers to tailor the care plan to the patient's needs and ensure effective treatment.
- Ongoing Feedback: Continuous feedback loops between patients and staff allow for adjustments to enhance the patient-centered approach.
Unexpected Discoveries: An unforeseen outcome of bedside rounding was the enthusiastic response from the WWH team, showcasing a departure from typical resistance to change. Staff members embraced the initiative, recognizing its potential to improve communication and patient care.
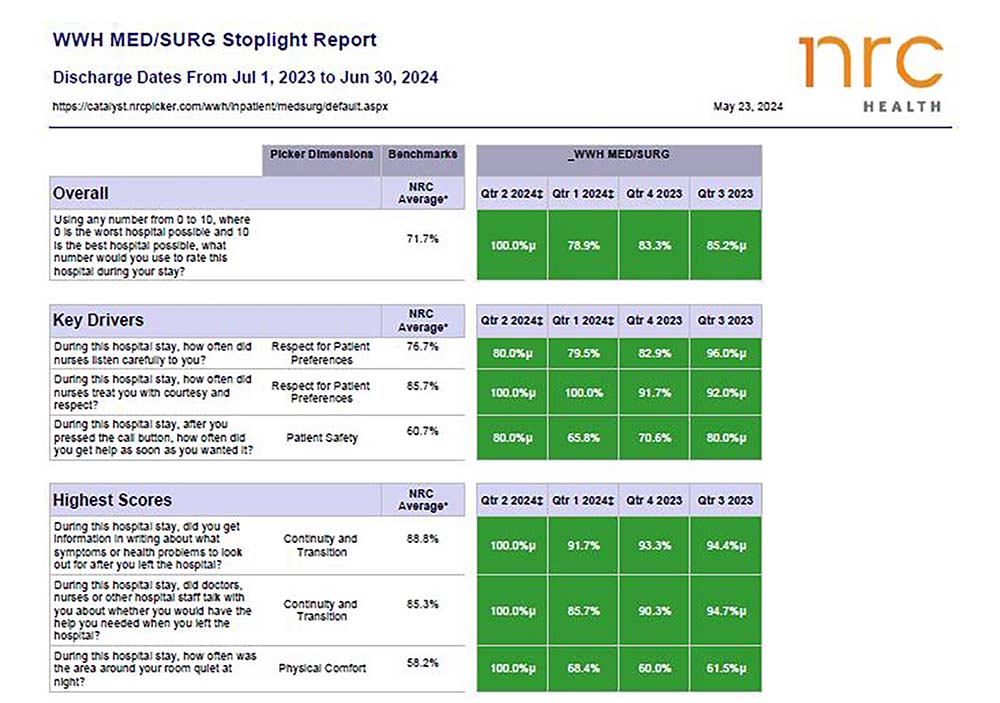
Data Points and Impact: Key Drivers:
- Improved Nurse and Provider Communication, including nurses listening to providers who explained things clearly.
- Patient preferences were acknowledged during their hospital stay.
Supporting Patient Comments:
- Patients and their caregivers expressed appreciation for being included in care planning, feeling heard, and better prepared to manage their health after discharge.
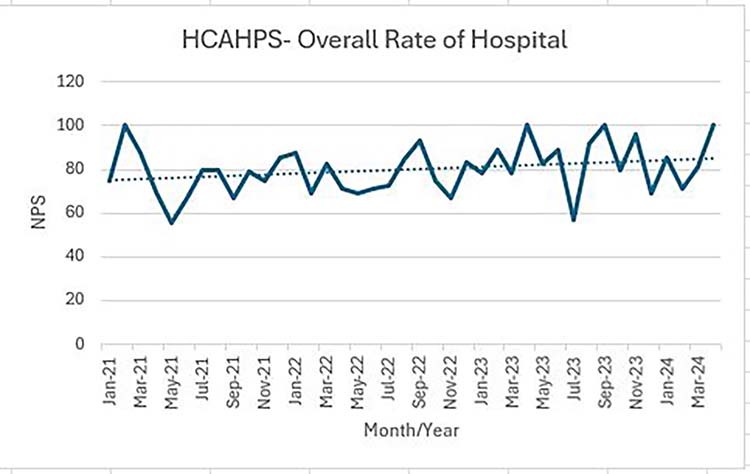
HCAHPS Results:
- Significant improvement in HCAHPS scores, reflecting enhanced patient engagement and satisfaction and feeling better informed.
Employee Engagement:
- High employee engagement scores were recorded, reflecting staff feeling valued, boosting morale, and their sense of commitment to excellent patient care.
- The nursing team identified a need for improvement in communication and proactively voiced their concerns, demonstrating their dedication to providing exceptional patient care.
Efficiency and Safety:
- Reduced need for multiple communications has enhanced efficiency and patient safety.
- Streamlined communication processes not only save time but also decrease the probability of errors or misunderstandings, thereby enhancing patient safety and effectiveness of care.
- Decreased readmission rates by 3% compared to the previous two years, supporting the effectiveness of the new process.
Conclusion: Bedside interdisciplinary rounding at WWH has emerged as a valuable practice, elevating communication, patient-centered care, and overall outcomes. By involving patients in care discussions and addressing communication barriers, WWH has witnessed improvements in patient satisfaction, staff engagement, and care efficiency. This approach not only meets immediate patient needs but also lays the groundwork for ongoing healthcare improvements.