Vol. 68, Issue 19
View more issues of The Valued Voice
Sign Up for WHA's Newsletter
Click here to view past issues
IN THIS ISSUE
- New AHA Report - Economic Pressures Facing Hospitals Threaten Access to Care
- Guest Column: The Disruptors Are Getting Disrupted — 5 Takeaways
- Gov. Evers Celebrates Wisconsin Hospitals in National Hospital Week Proclamation
- House Committee Advances Key Health Care Extensions
- Wisconsin Quality Residency 2024-2025 Kickoff on May 8
- Deadline this Week - WHA Foundation 2024 Clinical Simulation Lab Scholarship Application
EDUCATION EVENTS
Feb. 25, 2026
2026 Advocacy DayMar. 4, 2026
Spring 2026 Annual Survey TrainingMar. 5, 2026
Operational Vacancy: An Effective Tool for Workforce PlanningClick here to view education event calendar
View more issues of The Valued Voice
Sign Up for WHA's Newsletter
Thursday, May 9, 2024
New AHA Report - Economic Pressures Facing Hospitals Threaten Access to Care
On May 2, the American Hospital Association (AHA) released a new report highlighting how hospitals and health systems continue to face significant economic pressure on a number of fronts. These include escalating operating costs, increased demand for higher acuity care, workforce shortages, fractures in the supply chain, high levels of inflation, inadequate government reimbursement and administrative burden imposed by inappropriate commercial health insurer practices.
 “As this report clearly highlights, increased expenses, workforce challenges, and growing administrative burden are unsustainable and creating headwinds and obstacles that threaten access to care for millions of Americans,” said AHA President and CEO Rick Pollack in the AHA press release announcing the report.
“As this report clearly highlights, increased expenses, workforce challenges, and growing administrative burden are unsustainable and creating headwinds and obstacles that threaten access to care for millions of Americans,” said AHA President and CEO Rick Pollack in the AHA press release announcing the report.
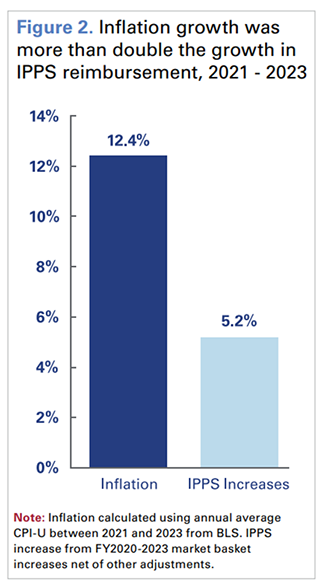
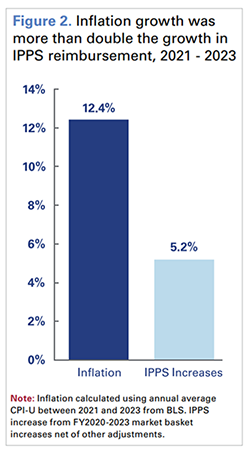
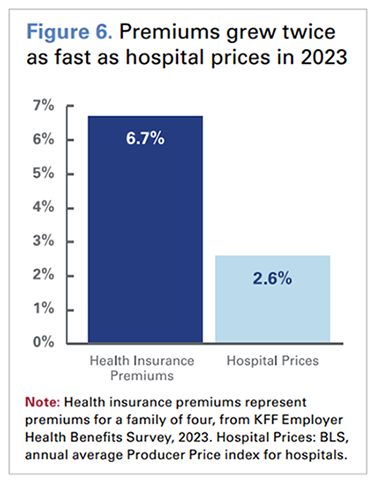
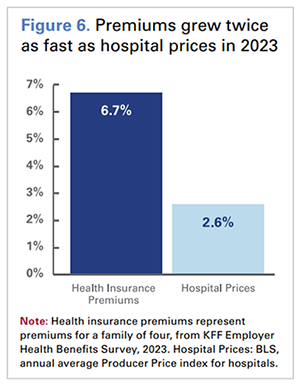
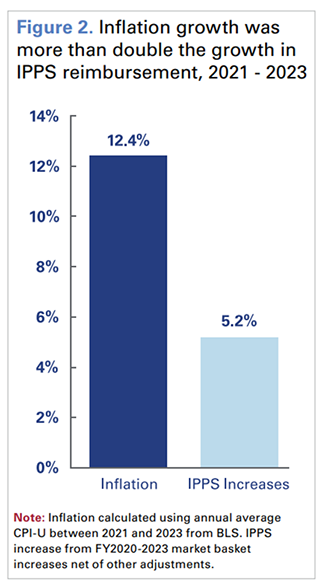
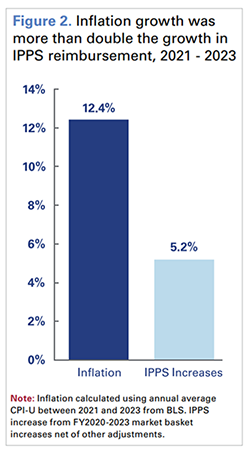
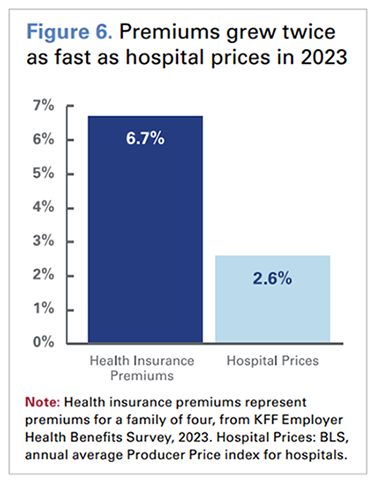
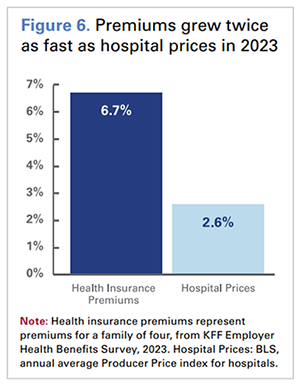
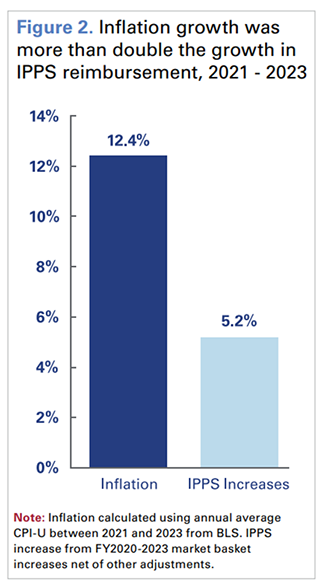
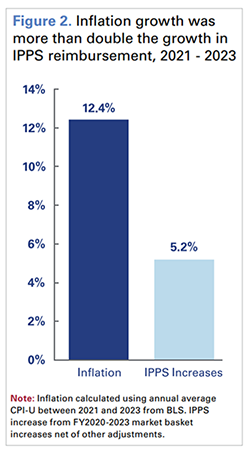
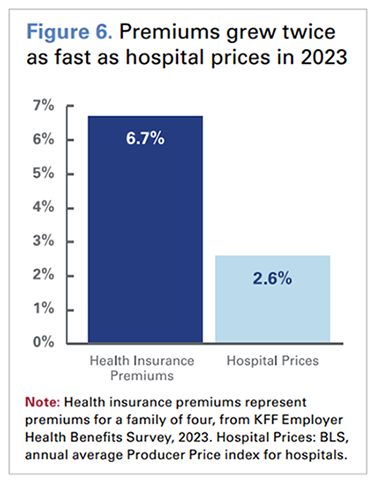
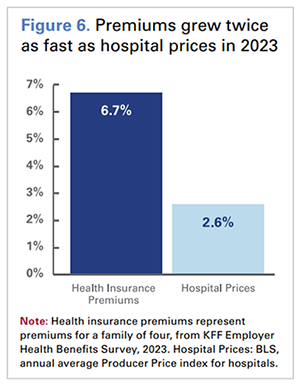
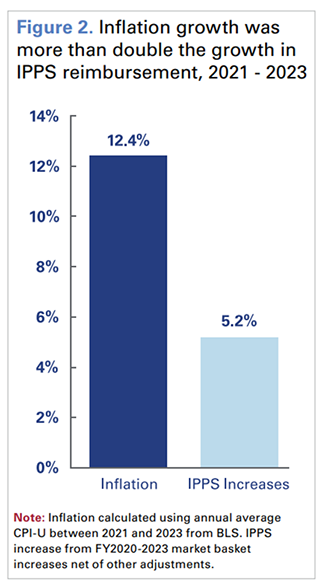
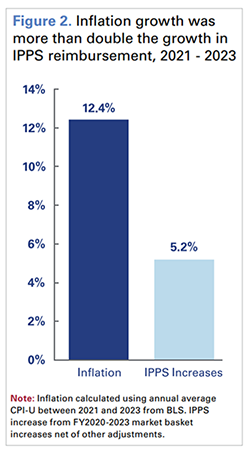
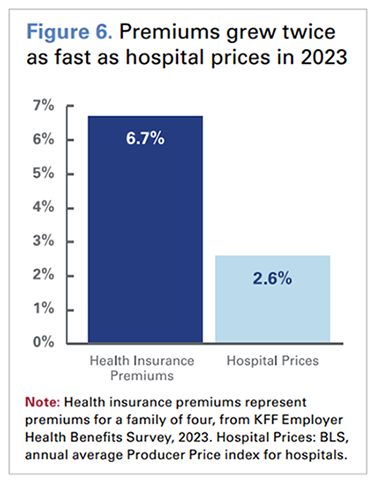
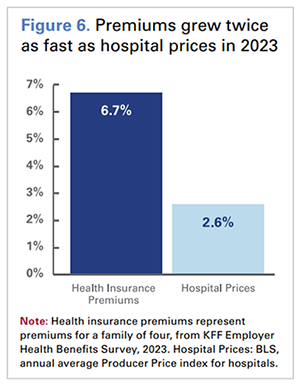
The ongoing challenges faced by hospitals are demonstrated by some troubling statistics. While inflation growth from 2021-2023 reached 12.4%, Medicare reimbursement grew by less than half of that – just 5.2%. Days cash on hand for hospitals and health systems has declined by nearly 30% since the start of 2022. Payments for inpatient behavior health services were on average 34% below cost across all payers. A 2023 study by Premier found that hospitals are spending just under $20 billion annually in appealing insurer denials, more than half of which was wasted on claims that should have been paid initially. At the same time, health insurance premiums grew twice as fast as hospital prices. Hospital labor costs, which on average account for 60% of expenses, increased by more than $42.5 billion between 2021 and 2023.
 As indicated in the report, “…The hospital field is still far from where it needs to be to meet the demand for care, invest in new and promising technologies and interventions, and stand ready for the next health care crisis.”
As indicated in the report, “…The hospital field is still far from where it needs to be to meet the demand for care, invest in new and promising technologies and interventions, and stand ready for the next health care crisis.”
The AHA continues to urge policymakers to support resources that will allow hospitals and health systems to continue providing 24/7 care to patients by rejecting Medicare and Medicaid cuts such as harmful site-neutral proposals; supporting the health care workforce; protecting the 340B programs and reining in the cost of drugs; taking actions to hold commercial insurers accountable for inappropriate practices that delay, deny and disrupt care; and support for enhancing cybersecurity.
 “As this report clearly highlights, increased expenses, workforce challenges, and growing administrative burden are unsustainable and creating headwinds and obstacles that threaten access to care for millions of Americans,” said AHA President and CEO Rick Pollack in the AHA press release announcing the report.
“As this report clearly highlights, increased expenses, workforce challenges, and growing administrative burden are unsustainable and creating headwinds and obstacles that threaten access to care for millions of Americans,” said AHA President and CEO Rick Pollack in the AHA press release announcing the report. The ongoing challenges faced by hospitals are demonstrated by some troubling statistics. While inflation growth from 2021-2023 reached 12.4%, Medicare reimbursement grew by less than half of that – just 5.2%. Days cash on hand for hospitals and health systems has declined by nearly 30% since the start of 2022. Payments for inpatient behavior health services were on average 34% below cost across all payers. A 2023 study by Premier found that hospitals are spending just under $20 billion annually in appealing insurer denials, more than half of which was wasted on claims that should have been paid initially. At the same time, health insurance premiums grew twice as fast as hospital prices. Hospital labor costs, which on average account for 60% of expenses, increased by more than $42.5 billion between 2021 and 2023.
 As indicated in the report, “…The hospital field is still far from where it needs to be to meet the demand for care, invest in new and promising technologies and interventions, and stand ready for the next health care crisis.”
As indicated in the report, “…The hospital field is still far from where it needs to be to meet the demand for care, invest in new and promising technologies and interventions, and stand ready for the next health care crisis.” The AHA continues to urge policymakers to support resources that will allow hospitals and health systems to continue providing 24/7 care to patients by rejecting Medicare and Medicaid cuts such as harmful site-neutral proposals; supporting the health care workforce; protecting the 340B programs and reining in the cost of drugs; taking actions to hold commercial insurers accountable for inappropriate practices that delay, deny and disrupt care; and support for enhancing cybersecurity.
Vol. 68, Issue 19
Thursday, May 9, 2024
New AHA Report - Economic Pressures Facing Hospitals Threaten Access to Care
On May 2, the American Hospital Association (AHA) released a new report highlighting how hospitals and health systems continue to face significant economic pressure on a number of fronts. These include escalating operating costs, increased demand for higher acuity care, workforce shortages, fractures in the supply chain, high levels of inflation, inadequate government reimbursement and administrative burden imposed by inappropriate commercial health insurer practices.
 “As this report clearly highlights, increased expenses, workforce challenges, and growing administrative burden are unsustainable and creating headwinds and obstacles that threaten access to care for millions of Americans,” said AHA President and CEO Rick Pollack in the AHA press release announcing the report.
“As this report clearly highlights, increased expenses, workforce challenges, and growing administrative burden are unsustainable and creating headwinds and obstacles that threaten access to care for millions of Americans,” said AHA President and CEO Rick Pollack in the AHA press release announcing the report.
The ongoing challenges faced by hospitals are demonstrated by some troubling statistics. While inflation growth from 2021-2023 reached 12.4%, Medicare reimbursement grew by less than half of that – just 5.2%. Days cash on hand for hospitals and health systems has declined by nearly 30% since the start of 2022. Payments for inpatient behavior health services were on average 34% below cost across all payers. A 2023 study by Premier found that hospitals are spending just under $20 billion annually in appealing insurer denials, more than half of which was wasted on claims that should have been paid initially. At the same time, health insurance premiums grew twice as fast as hospital prices. Hospital labor costs, which on average account for 60% of expenses, increased by more than $42.5 billion between 2021 and 2023.
 As indicated in the report, “…The hospital field is still far from where it needs to be to meet the demand for care, invest in new and promising technologies and interventions, and stand ready for the next health care crisis.”
As indicated in the report, “…The hospital field is still far from where it needs to be to meet the demand for care, invest in new and promising technologies and interventions, and stand ready for the next health care crisis.”
The AHA continues to urge policymakers to support resources that will allow hospitals and health systems to continue providing 24/7 care to patients by rejecting Medicare and Medicaid cuts such as harmful site-neutral proposals; supporting the health care workforce; protecting the 340B programs and reining in the cost of drugs; taking actions to hold commercial insurers accountable for inappropriate practices that delay, deny and disrupt care; and support for enhancing cybersecurity.
 “As this report clearly highlights, increased expenses, workforce challenges, and growing administrative burden are unsustainable and creating headwinds and obstacles that threaten access to care for millions of Americans,” said AHA President and CEO Rick Pollack in the AHA press release announcing the report.
“As this report clearly highlights, increased expenses, workforce challenges, and growing administrative burden are unsustainable and creating headwinds and obstacles that threaten access to care for millions of Americans,” said AHA President and CEO Rick Pollack in the AHA press release announcing the report. The ongoing challenges faced by hospitals are demonstrated by some troubling statistics. While inflation growth from 2021-2023 reached 12.4%, Medicare reimbursement grew by less than half of that – just 5.2%. Days cash on hand for hospitals and health systems has declined by nearly 30% since the start of 2022. Payments for inpatient behavior health services were on average 34% below cost across all payers. A 2023 study by Premier found that hospitals are spending just under $20 billion annually in appealing insurer denials, more than half of which was wasted on claims that should have been paid initially. At the same time, health insurance premiums grew twice as fast as hospital prices. Hospital labor costs, which on average account for 60% of expenses, increased by more than $42.5 billion between 2021 and 2023.
 As indicated in the report, “…The hospital field is still far from where it needs to be to meet the demand for care, invest in new and promising technologies and interventions, and stand ready for the next health care crisis.”
As indicated in the report, “…The hospital field is still far from where it needs to be to meet the demand for care, invest in new and promising technologies and interventions, and stand ready for the next health care crisis.” The AHA continues to urge policymakers to support resources that will allow hospitals and health systems to continue providing 24/7 care to patients by rejecting Medicare and Medicaid cuts such as harmful site-neutral proposals; supporting the health care workforce; protecting the 340B programs and reining in the cost of drugs; taking actions to hold commercial insurers accountable for inappropriate practices that delay, deny and disrupt care; and support for enhancing cybersecurity.
IN THIS ISSUE
- New AHA Report - Economic Pressures Facing Hospitals Threaten Access to Care
- Guest Column: The Disruptors Are Getting Disrupted — 5 Takeaways
- Gov. Evers Celebrates Wisconsin Hospitals in National Hospital Week Proclamation
- House Committee Advances Key Health Care Extensions
- Wisconsin Quality Residency 2024-2025 Kickoff on May 8
- Deadline this Week - WHA Foundation 2024 Clinical Simulation Lab Scholarship Application

