Vol. 68, Issue 31
View more issues of The Valued Voice
Sign Up for WHA's Newsletter
Click here to view past issues
IN THIS ISSUE
- Wisconsin Employers Saved Over $1 Billion in Worker’s Comp Premiums Since 2017
- WHA to Sen. Baldwin: Focus Should be on Keeping Hospitals Open Rather than Regulating Closures
- Southern and Western Region Host DHS Leader at Annual Dinner
- HealthPartners to Exit UnitedHealthcare's Medicare Advantage Network Over Payment Issues
- WHA-Crafted Training Grant Applications Now Open
- New Coalition Report on Value of 24/7 Care Provided by Hospitals
- August Fast Facts: Heat-Related Illnesses
EDUCATION EVENTS
Feb. 23, 2026
Nursing Services Conditions of ParticipationFeb. 25, 2026
2026 Advocacy DayMar. 5, 2026
Operational Vacancy: An Effective Tool for Workforce PlanningClick here to view education event calendar
View more issues of The Valued Voice
Sign Up for WHA's Newsletter
Thursday, August 1, 2024
HealthPartners to Exit UnitedHealthcare's Medicare Advantage Network Over Payment Issues
HealthPartners, a major health care provider based in Bloomington, MN that has hospitals in Amery, Hudson and New Richmond, Wisconsin, has announced its decision to leave UnitedHealthcare's Medicare Advantage network starting next year. As reported by the Star Tribune on July 23, HealthPartners says the decision stems from the insurer’ high rates of coverage denials and payment delays, which adversely affect patient care. Approximately 30,000 patients will be notified of this change through letters being sent out this week.
The health system highlights that UnitedHealthcare's denial rate is up to ten times higher than other insurers in the market. While UnitedHealth refutes these claims, HealthPartners says that these practices cause unnecessary waits and interfere with appropriate care for seniors.
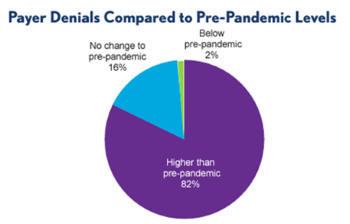
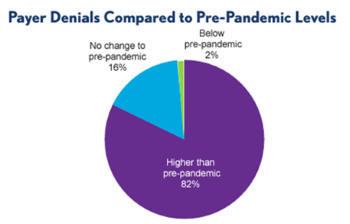
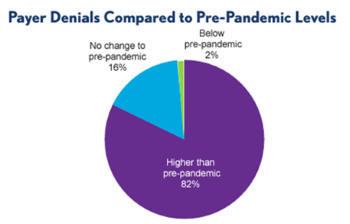
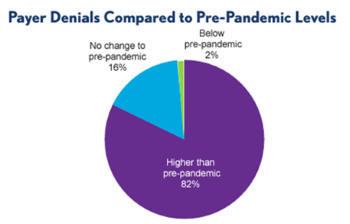
Insurer denials are on the rise across the country, according to a report released in March 2024 by the Healthcare Financial Management Association (HFMA) and Eliciting Insights, a health care strategy and market research company. The report cites 82% of health systems are experiencing higher payer denials than pre-pandemic levels, and 84% of hospitals and health systems report lower reimbursement from payers as the top cause of margin pressure.
"As we witness an increasing trend of insurer denials and delayed payments across the health care industry, HealthPartners' decision to exit UnitedHealthcare's Medicare Advantage network highlights the pressing need for fair and timely reimbursement practices,” said WHA President & CEO Eric Borgerding. “The impact of these delays and denials on patient care cannot be understated.”
HealthPartners’ move reflects a broader frustration among health systems nationwide with payers’ burdensome prior authorization requirements and increased denial rates. According to the report, 19% of health systems have stopped accepting a Medicare Advantage plan and 61% are planning to or are considering it.
HealthPartners, which is Minnesota’s second-largest nonprofit health care group, includes major hospitals and clinics in the Twin Cities area and three hospitals Wisconsin. This move follows a similar decision last summer when HealthPartners announced it would leave Humana's Medicare Advantage network in 2024.
Source, charts: https://www.hfma.org/wp-content/uploads/2024/03/Overview-2024-CFO-Pain-Points-Study.pdf
The health system highlights that UnitedHealthcare's denial rate is up to ten times higher than other insurers in the market. While UnitedHealth refutes these claims, HealthPartners says that these practices cause unnecessary waits and interfere with appropriate care for seniors.
Insurer denials are on the rise across the country, according to a report released in March 2024 by the Healthcare Financial Management Association (HFMA) and Eliciting Insights, a health care strategy and market research company. The report cites 82% of health systems are experiencing higher payer denials than pre-pandemic levels, and 84% of hospitals and health systems report lower reimbursement from payers as the top cause of margin pressure.
"As we witness an increasing trend of insurer denials and delayed payments across the health care industry, HealthPartners' decision to exit UnitedHealthcare's Medicare Advantage network highlights the pressing need for fair and timely reimbursement practices,” said WHA President & CEO Eric Borgerding. “The impact of these delays and denials on patient care cannot be understated.”
HealthPartners’ move reflects a broader frustration among health systems nationwide with payers’ burdensome prior authorization requirements and increased denial rates. According to the report, 19% of health systems have stopped accepting a Medicare Advantage plan and 61% are planning to or are considering it.
HealthPartners, which is Minnesota’s second-largest nonprofit health care group, includes major hospitals and clinics in the Twin Cities area and three hospitals Wisconsin. This move follows a similar decision last summer when HealthPartners announced it would leave Humana's Medicare Advantage network in 2024.
Source, charts: https://www.hfma.org/wp-content/uploads/2024/03/Overview-2024-CFO-Pain-Points-Study.pdf
Vol. 68, Issue 31
Thursday, August 1, 2024
HealthPartners to Exit UnitedHealthcare's Medicare Advantage Network Over Payment Issues
HealthPartners, a major health care provider based in Bloomington, MN that has hospitals in Amery, Hudson and New Richmond, Wisconsin, has announced its decision to leave UnitedHealthcare's Medicare Advantage network starting next year. As reported by the Star Tribune on July 23, HealthPartners says the decision stems from the insurer’ high rates of coverage denials and payment delays, which adversely affect patient care. Approximately 30,000 patients will be notified of this change through letters being sent out this week.
The health system highlights that UnitedHealthcare's denial rate is up to ten times higher than other insurers in the market. While UnitedHealth refutes these claims, HealthPartners says that these practices cause unnecessary waits and interfere with appropriate care for seniors.
Insurer denials are on the rise across the country, according to a report released in March 2024 by the Healthcare Financial Management Association (HFMA) and Eliciting Insights, a health care strategy and market research company. The report cites 82% of health systems are experiencing higher payer denials than pre-pandemic levels, and 84% of hospitals and health systems report lower reimbursement from payers as the top cause of margin pressure.
"As we witness an increasing trend of insurer denials and delayed payments across the health care industry, HealthPartners' decision to exit UnitedHealthcare's Medicare Advantage network highlights the pressing need for fair and timely reimbursement practices,” said WHA President & CEO Eric Borgerding. “The impact of these delays and denials on patient care cannot be understated.”
HealthPartners’ move reflects a broader frustration among health systems nationwide with payers’ burdensome prior authorization requirements and increased denial rates. According to the report, 19% of health systems have stopped accepting a Medicare Advantage plan and 61% are planning to or are considering it.
HealthPartners, which is Minnesota’s second-largest nonprofit health care group, includes major hospitals and clinics in the Twin Cities area and three hospitals Wisconsin. This move follows a similar decision last summer when HealthPartners announced it would leave Humana's Medicare Advantage network in 2024.
Source, charts: https://www.hfma.org/wp-content/uploads/2024/03/Overview-2024-CFO-Pain-Points-Study.pdf
The health system highlights that UnitedHealthcare's denial rate is up to ten times higher than other insurers in the market. While UnitedHealth refutes these claims, HealthPartners says that these practices cause unnecessary waits and interfere with appropriate care for seniors.
Insurer denials are on the rise across the country, according to a report released in March 2024 by the Healthcare Financial Management Association (HFMA) and Eliciting Insights, a health care strategy and market research company. The report cites 82% of health systems are experiencing higher payer denials than pre-pandemic levels, and 84% of hospitals and health systems report lower reimbursement from payers as the top cause of margin pressure.
"As we witness an increasing trend of insurer denials and delayed payments across the health care industry, HealthPartners' decision to exit UnitedHealthcare's Medicare Advantage network highlights the pressing need for fair and timely reimbursement practices,” said WHA President & CEO Eric Borgerding. “The impact of these delays and denials on patient care cannot be understated.”
HealthPartners’ move reflects a broader frustration among health systems nationwide with payers’ burdensome prior authorization requirements and increased denial rates. According to the report, 19% of health systems have stopped accepting a Medicare Advantage plan and 61% are planning to or are considering it.
HealthPartners, which is Minnesota’s second-largest nonprofit health care group, includes major hospitals and clinics in the Twin Cities area and three hospitals Wisconsin. This move follows a similar decision last summer when HealthPartners announced it would leave Humana's Medicare Advantage network in 2024.
Source, charts: https://www.hfma.org/wp-content/uploads/2024/03/Overview-2024-CFO-Pain-Points-Study.pdf
IN THIS ISSUE
- Wisconsin Employers Saved Over $1 Billion in Worker’s Comp Premiums Since 2017
- WHA to Sen. Baldwin: Focus Should be on Keeping Hospitals Open Rather than Regulating Closures
- Southern and Western Region Host DHS Leader at Annual Dinner
- HealthPartners to Exit UnitedHealthcare's Medicare Advantage Network Over Payment Issues
- WHA-Crafted Training Grant Applications Now Open
- New Coalition Report on Value of 24/7 Care Provided by Hospitals
- August Fast Facts: Heat-Related Illnesses

