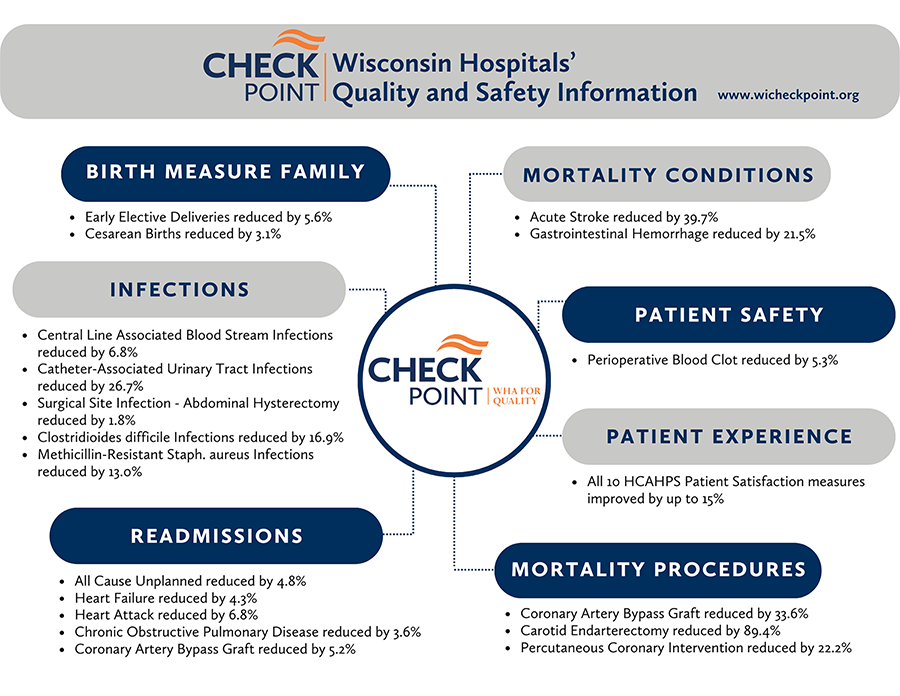
CheckPoint recently celebrated 20 years of being a nationwide leader providing transparent reporting of more than 40 quality metrics for Wisconsin hospitals. It fosters a culture of collaboration over competition and meets the demands from clinicians and consumers for information on the quality of care provided to patients and communities. Wisconsin hospitals can benchmark their progress against other hospitals in the state. In addition, the CheckPoint initiative has been a catalyst for Wisconsin hospitals to contact peers that are doing well in a clinical area to identify best practices which facilitates rapid improvement. The figure shows Wisconsin hospital outcomes data highlighting some of the measure improvements for recent 12 months of publicly available data:
In 2022, the Centers for Medicare & Medicaid Services (CMS) launched the CMS National Quality Strategy (NQS), a plan aimed at improving the quality and safety of health care for everyone, with a special focus on people from underserved and under-resourced communities. The CMS NQS builds on CMS’ efforts to improve health care quality for individuals across their lifespan and continuum of care by using all the Agency’s levers. Through its Hospital Value Based Purchasing Program, Hospital-Acquired Conditions Reduction Program and Hospital Readmissions Reduction Program, the Centers for Medicare & Medicaid Services (CMS) aims to improve the care provided by the nation’s hospitals and link Medicare payments to health care quality in the inpatient setting. In all three of these programs, Wisconsin hospitals improve year over year and routinely outperform other health care providers.
- Hospital Value Based Purchasing: Nationally, Wisconsin ranks in the top five (#5) of states achieving the highest monetary gains for goal achievement and improvement in this program.
- Hospital -Acquired Conditions: Seventy-three (73) percent of eligible Wisconsin hospitals do not receive a penalty in the HAC Reduction program.
- Hospital Readmission Reduction Program: For both FY 2023 and FY 2024, Wisconsin is ranked #15 nationally for states receiving the lowest dollar amount of penalties in this program.